Self-testing for cervical cancer could reduce cervical screening inequities for Māori, Pacific and Asian women, according to new research led by Massey University in partnership with Waitematā District Health Board and Auckland District Health Board.
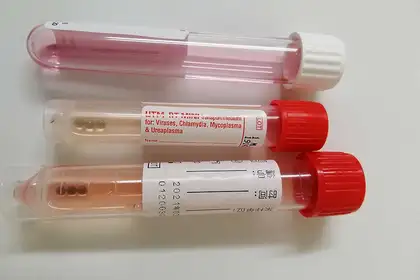
Cervical cancer is caused by the HPV (human papillomavirus). HPV can be picked up by a test (which, crucially, can also be a self-test) using a cotton swab. It is less invasive than the current test used in the National Cervical Screening Programme.
Since the introduction of the National Cervical Screening Programme, the death rate from cervical cancer in Aotearoa New Zealand has dropped by more than 70 per cent. Nonetheless, inequities in screening exist, with the majority of cervical cancer cases in Aotearoa occurring in women who have never been screened or are under-screened. Māori, Pacific and Asian women are the most under-served in the country, with the highest proportions of never and under-screened women.
Funded by the Health Research Council, the research was designed to reflect how self-testing would likely be implemented and whether it would improve coverage for women who experience the most barriers to health care.
The study randomised 3,553 women aged 30-69 into three groups – at home with a mailed-out HPV self-test kit, at a clinic with a self-test kit, or the current model of an in-clinic cervical screening performed by a health professional. The at-home mail-out group had the highest rate of participation.
Professor John Potter, from Massey University’s Research Centre for Hauora and Health, was the lead investigator for the study.
“This is the first New Zealand study to evaluate – in a randomised community trial – the effectiveness of mail-out HPV self-testing kits. Paired with clear international evidence, there is now a lot of support throughout Aotearoa to introduce this method of cervical screening on a national scale. This is especially important in light of the national health reforms announced this week,” Professor Potter says.
The findings show Māori women are nearly 10 times more likely to take a self-test at home than seek a standard cervical smear at a clinic. Pacific women were six times more likely and Asian women five times more likely.
Hei Āhuru Mōwai, National Māori Cancer Leadership co-Chair Dr Nina Scott was an advisor and co-author of the study.
“Wāhine Māori are dying of cervical cancer at a rate two to three times higher than other women. This study shows us that the HPV self-test could be used to dramatically improve access to cervical screening for wāhine Māori. Now is the time for change,” Dr Scott says.
Massey University senior lecturer in Molecular Pathology and co-author of the study, Dr Collette Bromhead, says the research was specifically designed to address local policy needs.
“The long-standing nature of our under-screening problem shows novel strategies are needed. As New Zealand transitions to primary HPV-based screening, there is an opportunity to introduce self-testing to directly address these inequities.”
The study also committed to a high level of follow-up, says Dr Karen Bartholomew, Director of Health Outcomes at Waitematā DHB and Auckland DHB.
“We know that HPV self-tests are empowering and less invasive for women but we also wanted to ensure that women who had a positive HPV test result felt comfortable and able to attend their follow-up appointments to get the full benefit of screening.
“We measured the support it took to achieve a 90 per cent follow-up rate because resources for equitable access to diagnosis and treatment will be an important requirement of an HPV primary screening programme too.”
Alongside other recent New Zealand evidence, the results for this study have been provided to the Ministry of Health to inform the future HPV primary screening programme.
Acceptability of human papillomavirus (HPV) self-sampling among never- and under-screened Indigenous and other minority women: a randomised three-arm community trial in Aotearoa New Zealand was carried out by:
Professor John Potter, Research Centre for Hauora and Health, Massey University and Fred Hutchinson Cancer Research Center, Seattle, United States
Dr Naomi Brewer, Research Centre for Hauora and Health, Massey University
Dr Karen Bartholomew, Waitematā District Health Board and Auckland District Health Board
Jane Grant, Waitematā District Health Board and Auckland District Health Board
Anna Maxwell, Waitematā District Health Board and Auckland District Health Board
Georgina McPherson, Waitematā District Health Board
Dr Helen Wihongi, Waitematā District Health Board and Auckland District Health Board
Dr Collette Bromhead, School of Health Sciences, Massey University
Dr Nina Scott, University of Auckland and Waikato District Health Board
Professor Sue Crengle, Department of Preventative and Social Medicine, University of Otago
Dr Sunia Foliaki, Research Centre for Hauora and Health, Massey University
Professor Chris Cunningham, Research Centre for Hauora and Health, Massey University
Professor Jeroen Douwes, Research Centre for Hauora and Health, Massey University
Findings are not yet peer-reviewed but are available on the preprint server medrXiv.